Heart disease doesn’t always announce itself with dramatic chest pain or collapse. Sometimes, it whispers — in the form of mild fatigue, shortness of breath, or occasional chest heaviness. Other times, it remains completely silent until tragedy strikes.
One of the biggest culprits behind this “silent killer” is blocked arteries, also known as coronary artery disease (CAD) — a condition that narrows or blocks the blood vessels supplying the heart. Without timely detection and treatment, it can lead to heart attacks, heart failure, or sudden cardiac death.
This article explores how artery blockages develop, the warning signs you should never ignore, and the cutting-edge diagnostic and treatment methods — including angiography and angioplasty — that can save lives when used early.
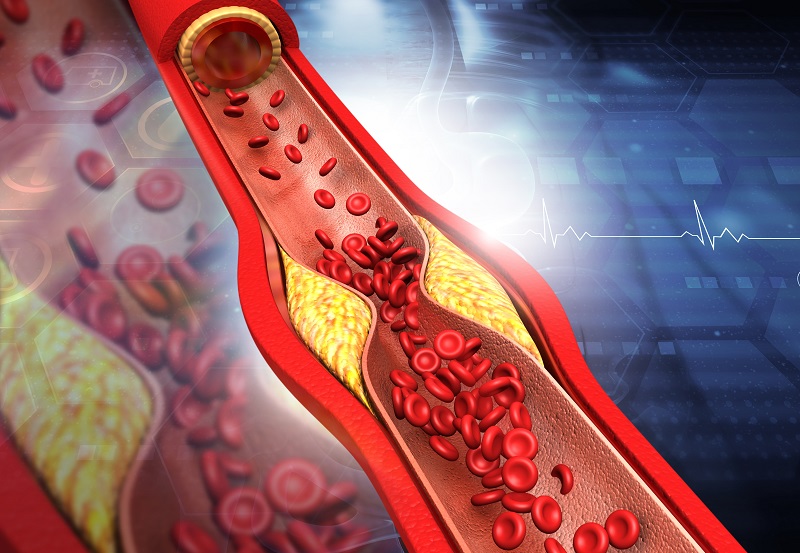
Your heart, the tireless engine of your body, pumps blood through a network of arteries that deliver oxygen and nutrients. Over time, these arteries can become clogged due to the buildup of fatty deposits known as plaques — a process called atherosclerosis.
Damage to Artery Walls:
Factors like high blood pressure, smoking, diabetes, or high cholesterol damage the inner lining of the arteries.
Cholesterol Accumulation:
Bad cholesterol (LDL) seeps into the damaged areas and gets trapped.
Plaque Formation:
The body’s immune response creates a mix of fat, calcium, and cellular waste that hardens into plaque.
Reduced Blood Flow:
As plaque grows, the arterial passage narrows — restricting the oxygen supply to the heart muscle.
Blockage or Rupture:
A plaque can rupture suddenly, triggering a blood clot that completely blocks blood flow — leading to a heart attack.
This process is slow, progressive, and often symptom-free — making it one of the deadliest stealth conditions.
Many people mistake the early symptoms of artery blockages for fatigue, acidity, or stress. But your heart might be sending subtle warning signals like:
Chest discomfort or tightness (especially during exertion)
Shortness of breath, even with mild activity
Pain radiating to the jaw, neck, shoulder, or back
Unexplained fatigue or weakness
Sweating, dizziness, or nausea
In diabetic patients and women, symptoms can be especially vague — like mild breathlessness or stomach discomfort — which often delays diagnosis. That’s why routine screening and preventive checks are critical even for those who feel “healthy.”
Early detection of arterial blockages dramatically improves treatment outcomes. One of the most important tools in this process is coronary angiography — a diagnostic test that visualizes the blood flow inside your coronary arteries in real time.
It’s a minimally invasive procedure that uses contrast dye and X-ray imaging to identify blockages in the arteries. A thin catheter is inserted through a blood vessel (usually in the wrist or groin) and guided to the coronary arteries. Once the dye is injected, doctors can see the exact location and severity of blockages on a live monitor.
Detects blockages before a heart attack occurs
Guides doctors in deciding whether angioplasty, stenting, or bypass surgery is needed
Helps assess heart function and blood flow efficiency
In recent years, advanced imaging technologies like OCT (Optical Coherence Tomography) and IVUS (Intravascular Ultrasound) have further enhanced accuracy — enabling cardiologists to visualize even the tiniest arterial changes.
The good news? Most arterial blockages are preventable. By making small but consistent lifestyle choices, you can dramatically reduce your risk.
Adopt a heart-healthy diet rich in:
Fresh fruits and vegetables
Whole grains
Lean proteins (fish, poultry, lentils)
Healthy fats (nuts, olive oil, avocados)
Avoid:
Processed foods
Sugary beverages
Trans fats and excessive salt
Just 30 minutes of moderate exercise a day can boost circulation, reduce cholesterol, and strengthen your heart.
Smoking accelerates plaque buildup and damages the arteries. Quitting immediately reduces your risk of heart disease — no matter how long you’ve smoked.
Chronic stress raises blood pressure and triggers inflammatory responses. Activities like yoga, meditation, and mindful breathing can protect both your heart and mind.
Diabetes and high cholesterol are silent accelerators of artery damage. Regular testing and timely medication can prevent long-term complications.
Even if you feel fine, annual check-ups — including blood pressure, lipid profile, ECG, and if indicated, a CT angiogram or stress test — can catch hidden risks early.
Modern cardiology has moved far beyond stethoscopes. Here are some of the key diagnostic tools that help detect arterial blockages early:
Detects abnormal electrical activity in the heart — often a first indicator of ischemia (restricted blood flow).
Evaluates how the heart responds to physical stress and helps identify early signs of coronary artery disease.
Uses sound waves to assess heart function and structural abnormalities.
A non-invasive imaging test that provides detailed 3D images of the coronary arteries — ideal for early screening in high-risk individuals.
The gold standard for diagnosing the exact location and severity of blockages.
Once a blockage is detected, treatment focuses on restoring blood flow and preventing future blockages.
Early or mild blockages can often be managed with:
Antiplatelet drugs (like aspirin)
Statins to lower cholesterol
Beta-blockers and ACE inhibitors to reduce heart strain
A minimally invasive procedure where a tiny balloon is inserted to open the blocked artery, followed by the placement of a stent (a small mesh tube) to keep it open.
Modern cardiology has also introduced zero-contrast angioplasty, especially for patients with kidney disease, minimizing dye exposure while ensuring precision.
In cases with multiple or severe blockages, surgeons create a new route for blood to flow — using vessels from other parts of the body.
For early-stage CAD, comprehensive programs combining diet, exercise, and stress management have shown measurable plaque regression.
Many heart patients share a common regret — “If only I had checked earlier.”
One 52-year-old executive, for instance, ignored his mild breathlessness as “stress.” A routine health check later revealed 90% blockage in a major coronary artery. A timely angioplasty not only saved his life but also helped him return to normalcy within days.
The lesson? Early diagnosis turns potential disasters into manageable conditions.
Even if you’re asymptomatic, consider cardiac screening if you have:
Family history of heart disease
Diabetes or high blood pressure
High cholesterol levels
Smoking or sedentary lifestyle
Chronic stress or obesity
Are above 40 years of age
Screening is especially vital for women, as their heart symptoms are often atypical and easily dismissed.
A widespread misconception is that absence of pain equals absence of disease.
But in the case of coronary artery disease, the opposite can be true. Nearly 40–50% of heart attacks occur in individuals who had no prior symptoms.
Heart health is not about reacting to pain — it’s about anticipating risk and acting before it’s too late.
Today’s cardiology blends precision with compassion. From AI-based risk prediction tools to ultra-low-radiation imaging and bio-absorbable stents, the field is evolving rapidly. But the foundation remains the same — prevention and early detection.
Hospitals and cardiac centers now offer comprehensive heart screening packages, including:
ECG + Echocardiogram
Lipid and sugar profile
CT or invasive angiography (if indicated)
Cardiologist consultation and lifestyle guidance
These tests, often completed within a few hours, can reveal what your body has been trying to hide for years.