Coronary Artery Bypass Grafting (CABG), commonly known as bypass surgery, is a significant procedure designed to improve blood flow to the heart. This surgery is typically recommended for patients with severe coronary artery disease (CAD). Understanding when to consider CABG is crucial for making informed health decisions. This blog will explore the conditions, symptoms, and evaluations that might lead to the recommendation of bypass surgery.
CAD occurs when the coronary arteries, which supply blood to the heart muscle, become narrowed or blocked due to a buildup of fatty deposits called plaques. This can lead to reduced blood flow and oxygen supply to the heart muscle, causing chest pain (angina), shortness of breath, or even heart attacks.
Patients experiencing severe, persistent symptoms that do not respond well to medication or lifestyle changes may need to consider CABG. These symptoms include:
CABG is often recommended when there are significant blockages in the coronary arteries, especially:
Patients who have undergone angioplasty or stenting but still have recurrent symptoms or complications may require CABG. This includes:
CABG may be considered for patients with weakened heart muscle (left ventricular dysfunction) due to CAD. Improving blood flow through bypass surgery can help restore heart function and reduce symptoms.
In some cases, CABG is performed as an emergency procedure, such as:
Before recommending CABG, a thorough evaluation is conducted, including:
A detailed review of the patient’s medical history, including risk factors, symptoms, and previous treatments, is essential. A physical examination helps assess overall health and suitability for surgery.
A team of cardiologists, cardiac surgeons, and other specialists collaborate to determine the best treatment approach based on the patient’s condition, preferences, and overall health.
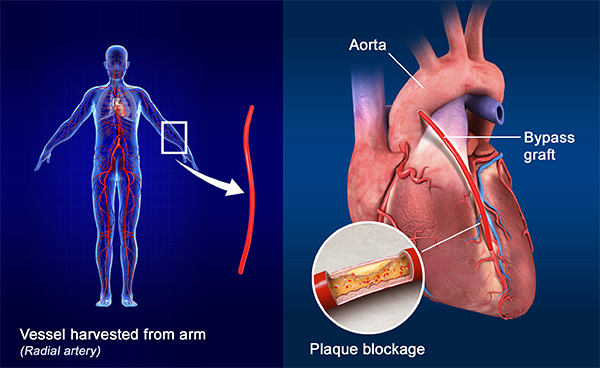
Q: What is CABG? A: Coronary Artery Bypass Grafting (CABG) is a surgical procedure to improve blood flow to the heart. It involves using a blood vessel from another part of the body to bypass a blocked or narrowed coronary artery.
Q: Why is CABG performed? A: CABG is performed to relieve symptoms of severe coronary artery disease (CAD), such as chest pain (angina), shortness of breath, and to reduce the risk of heart attack.
Q: When should I consider CABG? A: CABG should be considered if you have severe symptoms of CAD that do not respond to medication, significant blockages in coronary arteries, failed angioplasty or stenting, weakened heart muscle, or in emergency situations like a severe heart attack.
Q: How do I know if my symptoms are severe enough to require CABG? A: Symptoms that might indicate the need for CABG include intense chest pain, shortness of breath, and extreme fatigue that limits daily activities. Your doctor will evaluate your condition to determine if CABG is necessary.
Q: What tests are used to evaluate the need for CABG? A: Common tests include coronary angiography (to visualize blockages), stress tests (to measure heart response to exertion), and echocardiograms (to assess heart function and structure).
Q: How does my medical history impact the decision for CABG? A: Your medical history, including risk factors like high blood pressure, diabetes, and previous heart treatments, will be thoroughly reviewed to determine the suitability of CABG for your condition.
Q: What are the benefits of CABG? A: Benefits include improved blood flow to the heart, relief from severe symptoms, reduced risk of heart attack, and increased survival rates for patients with severe CAD.
Q: What are the risks associated with CABG? A: Risks include surgical complications like bleeding, infection, and adverse reactions to anesthesia, as well as a significant recovery period and the potential need for future reoperations.
Q: What is the recovery process like after CABG? A: Recovery involves a hospital stay, followed by a period of rehabilitation. Patients may need to make lifestyle changes, such as adopting a heart-healthy diet, quitting smoking, and engaging in regular physical activity.
Q: How long does it take to fully recover from CABG? A: Full recovery can take several weeks to months, depending on individual health, adherence to rehabilitation, and any complications that may arise.
Q: Are there alternatives to CABG? A: Alternatives include lifestyle changes, medication, and less invasive procedures like angioplasty and stenting. However, these may not be suitable for all patients, especially those with severe or complex CAD.
Q: How do angioplasty and stenting differ from CABG? A: Angioplasty and stenting involve opening narrowed arteries with a balloon and placing a stent to keep them open. CABG bypasses the blocked arteries using a blood vessel from another part of the body. Your doctor will recommend the best option based on your condition.
Q: How is the decision to undergo CABG made? A: The decision is made collaboratively by a team of healthcare providers, including cardiologists and cardiac surgeons, based on your symptoms, diagnostic test results, overall health, and personal preferences.
Q: What questions should I ask my doctor about CABG? A: Key questions include the reasons for recommending CABG, potential benefits and risks, recovery expectations, lifestyle changes post-surgery, and alternative treatment options.
Q: What follow-up care is required after CABG? A: Follow-up care includes regular check-ups with your cardiologist, adherence to prescribed medications, participation in cardiac rehabilitation programs, and maintaining a heart-healthy lifestyle.
Q: Can I return to normal activities after CABG? A: Most patients can return to normal activities gradually, but it is important to follow your doctor’s recommendations and participate in cardiac rehabilitation to ensure a safe and effective recovery.
If you have any further questions or need personalized advice, consult with your healthcare provider to discuss your specific situation and treatment options.